Medicine is a high-tech business—from the EMT with a defibrillator to the advanced equipment in the ICU. Timely repair is essential to health care. Delays in repair are dangerous as well as expensive. Hospitals cannot bill for procedures they cannot make while waiting on repair. A broken ventilator is useless in an emergency and a broken MRI machine delays diagnosis and care. Repair delayed is repair denied in times of emergency.
The COVID pandemic has brought these issues forward at the state and national level. Right to Repair requirements are being floated by state treasurers, attorneys general and executives. US Senator Ron Wyden has gone further — filing the Critical Medical Infrastructure Right to Repair Act.
Our template legislation has always been focused on blocking repair monopolies for anything with a chip, which includes medical equipment along with everything else. Valuable IP (copyrights, patents and trade secrets) is not stolen or proliferated by repair. Hackers do not get fresh access to cyber security through OEM provided service materials so sharing that same access already in the hands of authorized biomeds does not alter security risk.
Opponents routinely argue that the FDA requires reporting that isn’t the same as for hospitals. This is true and irrelevant. OEMs are regulated by the FDA and hospitals are regulated by CMS. Neither shares the same requirements other than patient care comes first, second, and third.
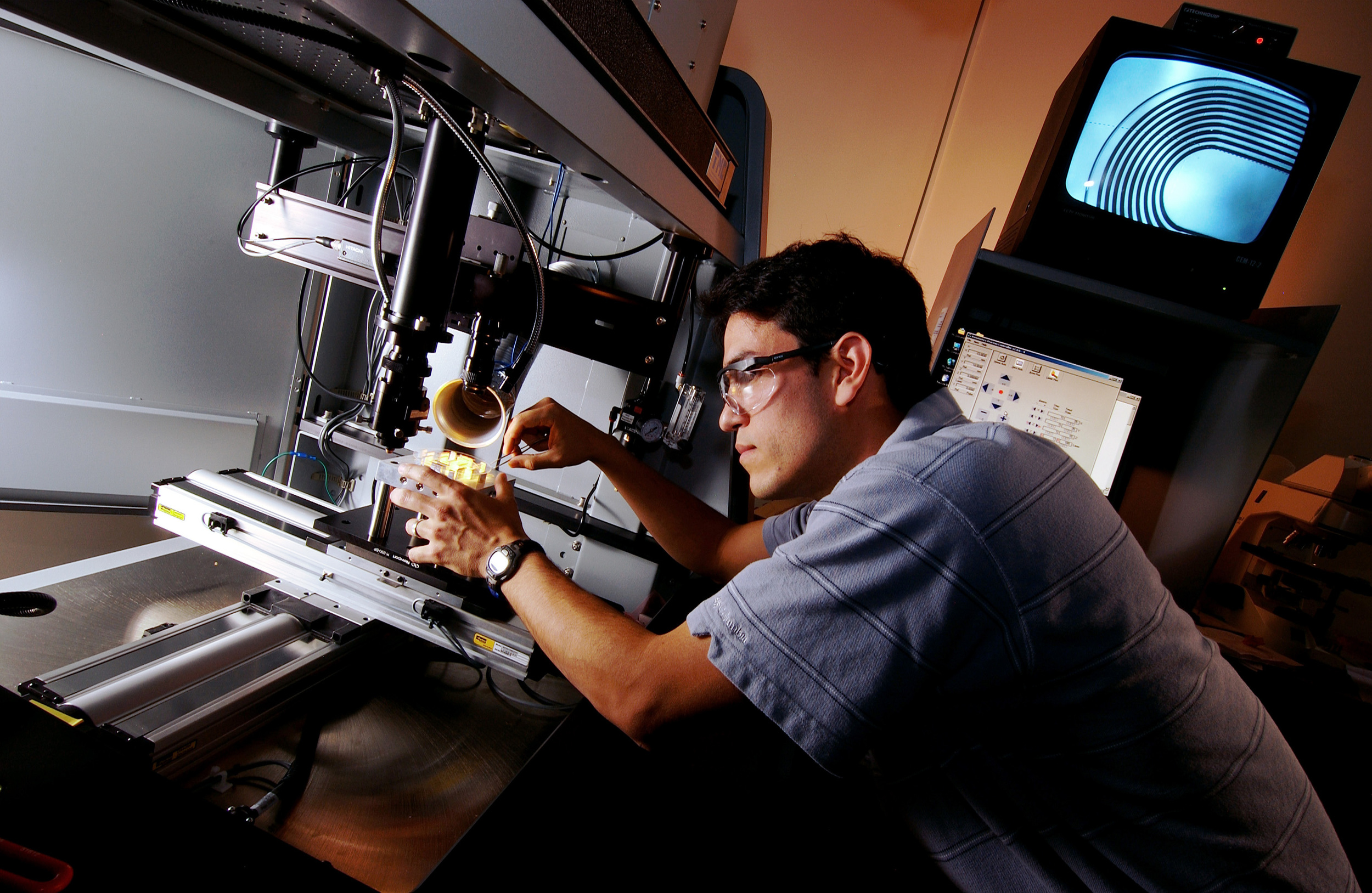
““Medical equipment repair technicians rely upon access to the same types of parts, tools, diagnostics, firmware and documentation as all other tech repair. We can share our skills and our voices as part of the entire repair community through repair.org.””
Hospitals and Clinics Need Access
Ahmad Nooristani was born in Afghanistan and immigrated to the United States with his family when he was 14 years old. Decades later, he opened a non-profit, free health clinic in San Luis Obispo, California—because he wanted to give back.
The doctors and nurses at the Noor Foundation Clinic rely on medical devices to help them diagnose and treat patients. And, because those machines cost thousands of dollars, Dr. Nooristani needs them to last for as long as possible. But everything breaks eventually.
But medical manufacturers won't share repair documentation with practitioners—even to free clinics like Dr. Nooristani's! They're presenting free clinics with a Hobbesian choice: pay exorbitant prices for the factory technician or go without the equipment.
In developing countries, broken hospital equipment is a life and death scenario.
“In some developing countries, up to 50% of the medical equipment is unusable at any given time. In some hospitals, up to 80% of their medical equipment is inoperative …”
Frank Weithoener is a well-regarded biomedical repair technician in Tanzania. He identifies five major barriers to medical device repair in developing countries:
No spare parts for repairs and maintenance
No technical manuals
Poorly trained biomedical technicians
No technical support from the manufacturers
Lack of awareness of the advantages of preventive maintenance
Since manufacturers weren't supporting the repair of their products, Frank decided to do it himself. He runs a website, Frank's Hospital Workshop, dedicated to training technicians. Unfortunately, Weyer, General Electric, and other manufacturers regularly send him legal threats and take-down notices demanding that he stop teaching people to repair life-critical medical equipment.
Take Action
Repair of critical hospital equipment is vital to the managing costs, and it's vital to providing patients with the care they need. The International Association of Medical Equipment Remarketers and Services (IAMERS) agrees. They've joined us in calling for wider access to repair information for hospitals.
More repair means better care.